How did the University of Queensland/CSL vaccine fail due to 'false positive' HIV tests? A vaccine expert explains
- Written by Adam Taylor, Early Career Research Leader, Emerging Viruses, Inflammation and Therapeutics Group, Menzies Health Institute Queensland, Griffith University
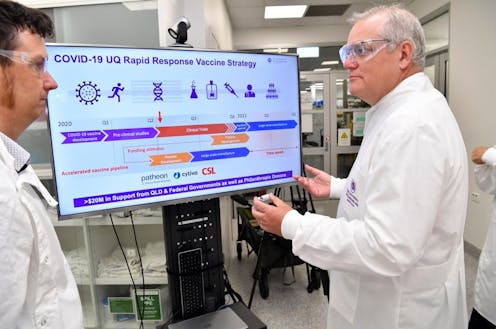
Australia’s hopes of producing a locally developed COVID-19 vaccine have been dashed with news today the University of Queensland/CSL vaccine would not proceed to further clinical trials.
However, unlike news about the Pfizer/BioNTech COVID vaccine earlier this week, there were no safety concerns with the UQ/CSL vaccine.
According to a statement to the Australian Stock Exchange (ASX) earlier today, CSL said participants in the phase 1 trial received “false positive” results to HIV tests. They were not infected with HIV, nor did the vaccine contain the entire HIV virus.
Rather, the vaccine’s signature “molecular clamp” technology was formulated with parts of an HIV protein. When injected, these prompted the production of antibodies that were picked up in a range of HIV tests. In other words, if the vaccine had been widely rolled out, this could lead many people to think they had HIV when they didn’t.
The news prompted the federal government to announce it had cancelled its agreement to supply the UQ/CSL vaccine, which was always contingent on successfully completing clinical trials.
Instead, the government will supply more doses of other vaccines, including 20 million extra doses of the University of Oxford/AstraZeneca vaccine, to be made by CSL.
The Oxford/AstraZeneca vaccine is the first COVID vaccine with published peer-reviewed results from phase 3 clinical trials, a significant milestone.
As well as the Oxford/AstraZeneca vaccine, existing arrangements are in place to supply Australians with the Pfizer/BioNTech and Novavax vaccines, should they prove safe and effective. That’s as well as vaccines available under the World Health Organisation-backed COVAX agreement.
Read more: Australia's just signed up for a shot at 9 COVID-19 vaccines. Here's what to expect
How could a COVID vaccine lead to a positive HIV test?
The UQ/CSL vaccine uses “molecular clamp” technology to present the coronavirus spike protein in the best orientation to elicit an immune response. In other words, the molecular clamp stops the spike protein from “wobbling about”. This more stable presentation is more likely to lead to a protective immune response.
The molecular clamp in UQ’s vaccine contains part of an HIV protein, a string of 80 amino acids. By itself, this is harmless and cannot cause an HIV infection or AIDS.
But there was always a theoretical possibility that once injected as part of the vaccine formulation, people’s immune systems would recognise it as “foreign” and raise antibodies against it. Until now, the research team thought the chance of that happening was low. And in its ASX statement CSL said people in the 216-person trial were fully informed of this possibility.
However, from what we’ve heard today, it’s clear that people’s immune systems did recognise the HIV protein fragment in the molecular clamp.
Had we rolled out this vaccine on a wider scale, we would have seen many more “false positive” HIV tests. This would have meant unnecessary anxiety while people sought further clarification about their HIV status.
It would also have undermined the public’s confidence in the COVID vaccination program. You have to have the public on board. So by acting early to clearly communicate concerns, the researchers have acted appropriately. And this should reinforce the public’s confidence in Australia’s COVID vaccination program, due to start from March 2021.
Read more: What will Australia's COVID vaccination program look like? 4 key questions answered
Is this the end of UQ’s ‘molecular clamp’ technology?
This particular molecular clamp is unique to UQ. So while this particular type will not be used for future vaccines, it’s likely the researchers will investigate and modify it to reduce the chance of any further HIV cross-reactivity.
I certainly don’t think it’s the end of this technology.
Read more: From adenoviruses to RNA: the pros and cons of different COVID vaccine technologies
So where does this leave us?
We’ve known all along that not all COVID-19 vaccines in early clinical trials would be successful. Safety issues or a lack of protection will halt some. But in this case, we had something different — a complication that would lead people to believe they had HIV when they didn’t, undermining people’s confidence in the COVID vaccine program.
That’s why it’s still important to pursue a broad portfolio of vaccine approaches and technologies. We don’t want to put all our eggs in one basket.
It’s also important to remember that even though the UQ/CSL vaccine will not proceed to late-stage clinical trials, phase 1 trials will continue, with results submitted for peer review in due course. That means researchers can analyse the results in more detail.
Authors: Adam Taylor, Early Career Research Leader, Emerging Viruses, Inflammation and Therapeutics Group, Menzies Health Institute Queensland, Griffith University



